Gastrointestinal (GI) issues
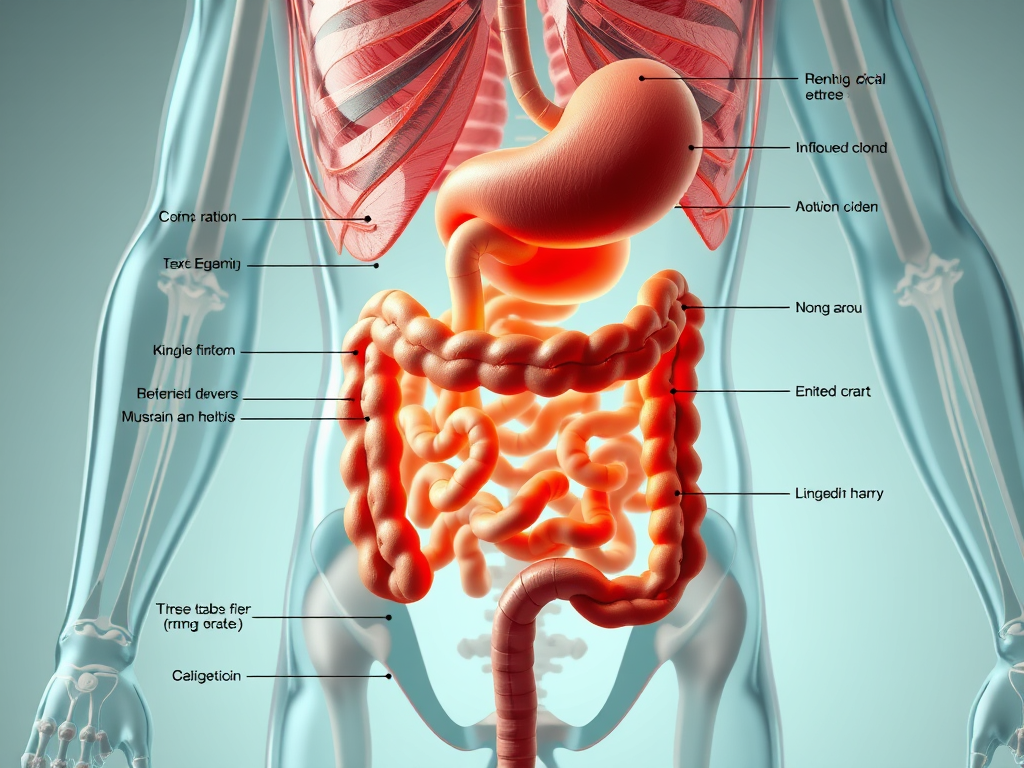
Gastrointestinal (GI) issues are widespread, affecting millions of individuals globally and significantly impacting their daily lives and overall well-being. The gastrointestinal tract, or digestive system, is a complex network of organs forming a long tube from the mouth to the anus, responsible for digesting food, absorbing nutrients and water, and expelling waste. When this intricate system malfunctions, it can lead to a diverse range of uncomfortable and sometimes severe symptoms. Understanding the different types of GI disorders, their common symptoms, and available treatments is crucial for effective management and maintaining a healthy digestive system.
Types of GI Disorders
Gastrointestinal diseases are broadly categorized into two main types: functional and structural.
Functional Gastrointestinal Disorders (FGIDs)
Functional gastrointestinal disorders are characterized by disruptions in the normal functioning of the digestive system without any visible physical or structural abnormalities that can be detected by standard diagnostic tests like blood tests or imaging. Instead, FGIDs are often attributed to a combination of abnormal muscle contractions, sensitive nerves, and dysfunction in the brain-gut axis—the communication network between the brain and the GI tract. These disorders can cause a variety of problems and signs, including bloating, constipation, diarrhea, gas, nausea, and, notably, irritable bowel syndrome (IBS) and uncomplicated gastroesophageal reflux disease (GERD).
Structural Gastrointestinal Disorders
In contrast, structural gastrointestinal disorders involve physical changes or visible abnormalities in the GI tract. These conditions can often be detected through imaging tests, blood work, or endoscopic procedures. Examples of structural GI diseases include tumors, strictures (narrowing of the tract), inflammatory bowel disease (IBD), hernias, diverticulosis and diverticulitis, peptic ulcers, gallstones, pancreatitis, complicated GERD (such as Barrett’s esophagus or esophageal strictures), and hemorrhoids.
Common GI Symptoms
The symptoms of GI diseases can vary widely depending on the specific condition and the affected part of the digestive system. However, many symptoms are common across various disorders and can sometimes be misinterpreted by both patients and healthcare providers. Some of the most frequently reported GI symptoms include:
- Abdominal pain or discomfort.
- Bloating and gas.
- Constipation (infrequent or difficult bowel movements, hard stools, straining, incomplete emptying).
- Diarrhea (loose or watery stools, increased frequency).
- Heartburn (a burning feeling in the chest or throat) and acid reflux.
- Nausea and vomiting.
- Blood in stool (red or black/tar-like).
- Unintentional weight loss.
- Difficulty swallowing (dysphagia) or painful swallowing (odynophagia).
Condition Spotlight Sections
Irritable Bowel Syndrome (IBS)
IBS is the most common functional GI disorder, affecting an estimated 5% (1 in 20) of the adult population in the United States and 10–15% in the developed world, with an average global prevalence of 11.2%. It is characterized by recurrent abdominal pain or discomfort in association with changes in bowel habits, which can include diarrhea (IBS-D), constipation (IBS-C), or alternating patterns (IBS-M). Symptoms often include an urge for bowel movements that don’t occur, a feeling of incomplete evacuation, and bloating, which may be relieved by bowel movements. In Western countries, IBS is typically twice as common in women as in men and usually appears before age 45.
The precise cause of IBS is unknown, but multiple factors are believed to contribute, including problems with the gut-brain axis, abnormal gut motility, visceral hypersensitivity (increased sensitivity to normal intestinal function), infections (such as small intestinal bacterial overgrowth or post-infectious IBS), neurotransmitter imbalances, genetic predispositions, and food sensitivities. Psychological stress, anxiety, and a sedentary lifestyle are also recognized triggers or exacerbating factors. Individuals with IBS often experience comorbidities such as GERD, fibromyalgia, headaches, backaches, depression, anxiety, sleep disorders, and sexual dysfunction.
Treatment for IBS focuses on managing symptoms and can include dietary changes, such as increasing soluble fiber or adopting a low-FODMAP diet (under dietitian supervision). Regular physical activity and stress management techniques like meditation or yoga are also beneficial. Medications like laxatives for constipation, antispasmodics, or low-dose antidepressants can help. Probiotics, which introduce beneficial bacteria, may also be recommended.
Gastroesophageal Reflux Disease (GERD)
GERD is a chronic condition characterized by severe acid reflux, where stomach acid repeatedly flows back up into the esophagus. This often occurs when the lower esophageal sphincter (LES), a muscle at the junction of the esophagus and stomach, is weak or malfunctions, allowing stomach contents to reflux.
The hallmark symptom of GERD is heartburn, a burning sensation in the chest or throat, which can worsen after eating spicy foods or caffeine, or when lying down too soon after meals. Other symptoms may include stomach pain, chest pain, nausea, and regurgitation (food coming back up into the throat or mouth). Factors contributing to GERD include diet, lifestyle habits, hiatal hernia, obesity, and pregnancy. Certain foods like chocolate, fried or fatty foods, and alcohol can weaken the LES.
Treatment for GERD typically begins with lifestyle modifications such as raising the head of the bed, eating smaller, more frequent meals, quitting smoking, and avoiding trigger foods and drinks. Over-the-counter antacids provide temporary relief by neutralizing stomach acid, while H2-blockers and more potent acid pump inhibitors (like omeprazole or lansoprazole) suppress acid production. In severe or resistant cases, antireflux surgery may be considered.
Inflammatory Bowel Disease (IBD)
IBD is an umbrella term for a group of chronic inflammatory conditions that cause inflammation throughout the digestive system and can lead to damage if left untreated. The exact cause of IBD is not fully understood, but it is believed that a genetic predisposition coupled with an altered immune response (possibly triggered by a virus or bacterium) leads to chronic inflammation in the intestinal wall. The onset of IBD often peaks during young adulthood.
The two main types of IBD are:
- Crohn’s Disease (CD): This chronic disease can affect any part of the GI tract, from the mouth to the anus, and typically involves all layers of the bowel wall. Common symptoms include abdominal pain and cramping (often in the lower right quadrant), weight loss, diarrhea (which can sometimes be bloody), and fatigue. Over time, inflammation can cause the intestinal wall to thicken, potentially leading to bowel obstruction and malnutrition.
- Ulcerative Colitis (UC): This chronic inflammatory disease primarily affects the large intestine (colon) and rectum, specifically the inner lining. Symptoms often include abdominal pain and cramping, bloody stools, diarrhea, and a constant, urgent need to have a bowel movement.
Treatment for IBD typically involves medications to reduce inflammation and suppress the immune system, such as sulfasalazine, prednisolone, mesalamine, metronidazole, and azathioprine. Dietary changes are also important, and a low-FODMAP diet may benefit some patients. In cases of severe damage or complications, surgery to remove diseased bowel may be necessary. While remission is possible, IBD is a lifelong condition requiring ongoing monitoring and treatment.
Diverticulitis
Diverticulitis occurs when small, bulging pouches (known as diverticula) that form in the lining of the lower colon become inflamed. Diverticulosis, the formation of these pouches, is common in older individuals in industrialized countries, and can also affect the small intestine.
Symptoms of diverticulitis include pain and cramping, typically in the lower left abdomen, often accompanied by nausea, vomiting, and fever. If left untreated, diverticulitis can lead to life-threatening complications.
Celiac Disease
Celiac disease is an autoimmune disorder where the consumption of gluten, a protein found in wheat, rye, and barley, triggers an immune response that damages the lining of the small intestine. This damage impairs the small intestine’s ability to properly absorb nutrients. Celiac disease is one of the most common digestive disorders, affecting approximately 1 in 133 people.
While some individuals with celiac disease may be asymptomatic, others experience a range of symptoms including diarrhea, constipation, fatigue, abdominal pain and bloating, gas, brain fog, rashes, joint pain, depression, and reproductive issues. Diagnosis typically involves a blood test to detect specific antibodies, followed by an intestinal biopsy to confirm damage to the small intestine lining. The only effective treatment for celiac disease is a strict, lifelong gluten-free diet. Untreated celiac disease can increase the risk of serious health problems such as osteoporosis, anemia, and certain cancers.
Gastroparesis
Gastroparesis, also known as delayed gastric emptying, is a disorder where the stomach takes too long to empty its contents into the small intestine. This condition is usually caused by damage to the nerves that control stomach muscle contractions.
Common symptoms include nausea, vomiting, and a feeling of uncomfortable fullness during or after a meal. Individuals with type 1 or type 2 diabetes are at an increased risk of developing gastroparesis, and certain medications can also be a contributing factor.
When to Seek Medical Advice
While many common GI symptoms like occasional stomachaches, bloating, constipation, or diarrhea may be temporary and resolve on their own, it is crucial to consult a healthcare provider for any persistent or severe gastrointestinal issues. Prompt medical attention is especially important if you experience any of the following “red-flag” symptoms:
- Symptoms that are severe or persist for more than a few days or weeks.
- Severe abdominal pain.
- Unintentional weight loss.
- Blood in your stool (bright red blood, dark blood, or black, tarry stools, resembling coffee grounds in vomit).
- Persistent or severe nausea and vomiting.
- Fever.
- Signs of dehydration (thirst, dry skin, fatigue, dizziness, less frequent urination, dark-colored urine).
- Heartburn not relieved by antacids. These symptoms could indicate a more serious underlying health condition, potentially including cancer or other emergencies that require immediate medical evaluation.
Diagnosis & Treatment Approaches
Accurately diagnosing gastrointestinal disorders often requires a comprehensive approach. This typically begins with a thorough medical history and physical examination. Based on initial findings, a healthcare provider may recommend various diagnostic tests:
- Laboratory Tests: Including blood tests (e.g., for celiac disease antibodies, anemia, inflammatory markers) and stool tests (e.g., for blood, infections).
- Imaging Studies: Such as abdominal ultrasound, CT (computerized axial tomography) scan, MRI, and upper or lower GI series (using X-rays with contrast).
- Endoscopic Procedures: Including colonoscopy, upper GI endoscopy, sigmoidoscopy, and capsule endoscopy, which allow direct visualization of the GI tract and collection of biopsies if needed.
- Breath Tests: For conditions like small intestinal bacterial overgrowth (SIBO) or lactose intolerance.
Treatment modalities for GI diseases are highly dependent on the specific condition, its underlying cause, and the severity of symptoms. Common approaches include:
- Lifestyle Changes: This is often the first line of defense and can include dietary modifications (e.g., increasing fiber, avoiding trigger foods, adopting a low-FODMAP diet), maintaining adequate hydration, engaging in regular physical activity, implementing stress management techniques (like meditation or yoga), practicing good hygiene, and avoiding smoking and excessive alcohol consumption.
- Medications: A wide array of prescription and over-the-counter medications are available, such as antacids, laxatives, antidiarrheals, antibiotics, anti-inflammatories, steroids, immune suppressors, acid pump inhibitors (for GERD), antidepressants (for certain FGIDs), antispasmodics, and probiotics. Specific agents like rifaximin and lubiprostone are used for IBS, and octreotide may manage certain bowel obstructions.
- Surgical Interventions: In some cases, surgical procedures may be necessary to address structural abnormalities, remove diseased tissue, repair hernias, or alleviate obstructions. Organ transplants are also an option for certain severe conditions.
- Emerging Therapies: Advances in molecular laboratory tests, artificial intelligence in gastrointestinal endoscopy, targeted and immunological oncological therapies, robotic surgery, bacteriophages for microbiome modulation, and mesenchymal stem cell therapy for IBD are continually improving diagnostic and treatment options.
A multidisciplinary team, including primary care physicians, gastroenterologists, nurse practitioners, physician assistants, nutritionists/dietitians, radiologists, surgeons, and oncologists, may be involved in the diagnosis and management of GI conditions.
Lifestyle & Gut–Brain Health
A significant and increasingly recognized concept in understanding GI issues is the gut-brain axis. This bidirectional communication system highlights how emotional and cognitive centers in the brain influence GI activity and immune function, and conversely, how the gut’s microbes can affect mood, cognition, and mental health. Psychosocial factors such as stress, anxiety, and depression are known to influence GI tract function, potentially exacerbating symptoms or contributing to the development and maintenance of functional GI disorders. For example, psychological stress can impair the gut’s mucosal barrier, allowing bacteria to migrate and cause pain or diarrhea.
The human gut microbiome—the vast community of microorganisms residing in the GI tract—also plays a crucial role in overall health and disease. Alterations in gut microbiota (dysbiosis) are associated with both intestinal symptoms and the psychiatric comorbidities often seen in individuals with IBS. The types of food consumed can significantly impact the microbiome. Strategies like stress management (e.g., meditation, yoga) and regular physical activity are not just for mental well-being but are fundamental to promoting a healthy gut and alleviating GI symptoms.
Conclusion
Gastrointestinal issues are a diverse group of conditions that can range from mild and temporary to chronic and debilitating, profoundly affecting quality of life. Recognizing common symptoms and understanding the distinction between functional and structural disorders is the first step toward effective management. Given the complexity and potential severity of many GI conditions, early diagnosis and appropriate treatment are paramount. If you experience persistent, severe, or “red-flag” gastrointestinal symptoms, it is always recommended to consult a healthcare professional. They can provide an accurate diagnosis, guide you through appropriate treatment options, and help you prioritize your gut health for a better quality of life.